Workplace Mental Health: How Experience Fuels Change
Some experiences are so profound they leave a lasting mark, shaping who we are and who we become. Our workplaces are the beneficiary of Stéphane’s experience.
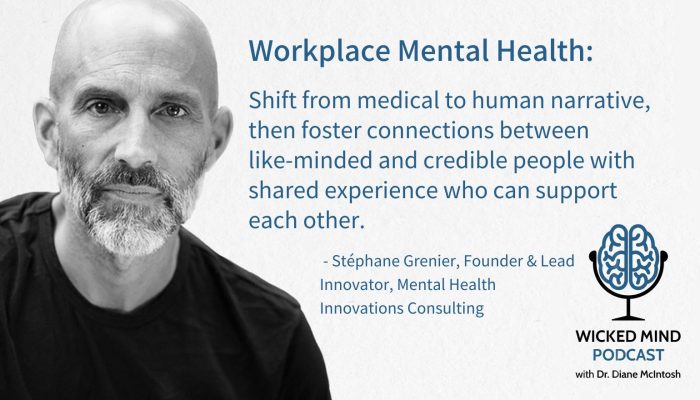
This blog features highlights from conversations about mental healthcare transformation on the Wicked Mind pod, hosted by Dr. Diane McIntosh. Listen to the full conversation with Stéphane Grenier and then explore others in the Wicked Mind series.
Stéphane Grenier, founder and lead innovator of Mental Health Innovations Consulting, has a story to share.
He starts with a fact. He has lived two lives. There is the life before he was deployed to Rwanda in 1994 as part of the Canadian peacekeeping mission during the genocide.
And there is his life after. “Arriving in Rwanda for me was the first day of the rest of my life.”
During his time in Rwanda, Grenier witnessed deaths and traumatic events. Upon his return home, he came to realize the profound impact that trauma can have. It also made him aware of how poorly understood and undertreated mental health really is.
After returning home from Rwanda in 1995, the now-retired lieutenant colonel was diagnosed with post-traumatic stress disorder (PTSD) and depression.
Six years later, his experiences and insights led him to coin the term Operational Stress Injury (OSI), a term that medicalizes a condition that is all too often dismissed. “It’s a term so lay people can wrap their minds around the notion that the brain is not immune to injury or illness,” he says.
He says that all too often physical injuries supersede psychological ones, particularly in organizations such as the military. And there’s little awareness that an injured brain changes over time and requires the same care and healing as a physical injury.
Grenier has become a notable mental health advocate, innovator, and entrepreneur and was appointed to the Order of Canada for his efforts.
He now routinely acts as a consultant to organizations on how best to implement mental health programs. He’s also released a book, After the War: Surviving PTSD and Changing Mental Health Culture.
“I don’t know how I would live my life today without bringing my experience and insights to help somebody else,” he says. “I know it makes a difference.”
Grenier’s goal is now to convince employers to adopt workplace mental health policies and approaches that harness the goodwill of employees to end the stigma around mental health issues.
He believes organizations need to take steps to ensure employees feel safe to discuss their mental health concerns and seek treatment in a non-judgmental environment.
Here are some of those steps:
Understand exactly how your mental health plan works
Grenier says that unless senior leaders are familiar with the organization’s policies, understand procedures and oversee the recruitment of individuals overseeing mental health initiatives, they can’t guarantee the outcome of mental health training. They need to have a robust understanding of their mental health program in order to guarantee its success. Once that happens, and the program is successfully launched, they can hand the reins to those staff members leading the mental health initiatives.
Have an effective peer support program
Grenier is a big proponent of peer support programs to help employees who are struggling with their mental health. Training and supporting peers is important, but Grenier emphasizes that selecting people and paying attention to which “bucket” you are in are critical to success. It’s not a one-stop solution.
Take an inventory: which bucket are you in?
Grenier talks about the three workplace mental health buckets that he finds organizations in.
Bucket one is the “poster and committee” bucket, focused on doing things that might give you a sense of action.
Bucket two is the belief that the only thing that can be helpful for mental health are clinicians like doctors, psychiatrists, psychologists.
Bucket three is where his heart and efforts lie – the “change the narrative” bucket. He is a passionate advocate for shifting a medical narrative to a human narrative, one that fosters connections between people, like-minded and credible people with shared experience who can create emotional resonance and support each other.
It’s not surprising that Stéphane and the team at Mental Health Innovations (MHI) work with organizations who can see beyond the limitations of a focus on either of the two first two buckets.
Rethink critical stress debriefings
A critical stress debriefing is a crisis intervention process commonly used by organizations, including law enforcement. During these sessions, employees relay what happened during a traumatic incident. Grenier says that new research indicates that these types of interventions can backfire and actually lead employees to relive the trauma they’ve experienced, leading them to develop PTSD at a later time. “There’s so much compelling evidence to say, ‘stop doing this,’” he says.
Harness the power of your team
Getting the buy-in of employees is instrumental in the success of a mental health program. This team approach can make other staffers feel less invisible – and more empowered to speak up and seek help. “[You] can crowdsource human benevolence from within your existing organization,” says Grenier. “They show up — all you need to do is give them an opportunity to be part of the solution and allow them to pay it forward in a safe way.”
“That’s how you change culture.”
Listen to my conversation with Stéphane Grenier on the Wicked Mind podcast>>
See also my post on 7 Ways Employers can do to Support Employee Mental Health
This blog post is part of a series looking at the state of our mental healthcare system and ways we can create sustainable change to improve quality and outcomes for anyone impacted by mental illness.
Understanding Panic Disorder: Symptoms, Treatment, Bravery in Asking for Help
Panic disorder, which affects 3.7% Canadians, is “fear gone wrong.” With appropriate therapy and medication, people with panic disorder can keep symptoms in check. Summary of “This is Panic Disorder”, Episode 6 of PSYCHEDUP Podcast.
Living with PTSD: A journey from trauma to healing
Post-traumatic stress disorder doesn’t just affect soldiers; it can affect anyone who has experienced trauma. But treatment can help. Chelan shares her story. Summary of “This is PTSD”, Episode 5 of the PSYCHEDUP Podcast.
Understanding Bipolar Disorder: The highs, the lows, and the road to equanimity
Bipolar disorder often hides behind depression, making diagnosis a challenge. Pauline navigated years of highs and lows before finding stability. Hear how finally receiving an accurate diagnosis and effective treatment can transform lives for people like Pauline. Summary of “This is Bipolar”, Episode 4 of the PSYCHEDUP Podcast.
