Leadership in action with Louise Bradley

This blog features highlights from conversations about mental healthcare transformation on the Wicked Mind pod, hosted by Dr. Diane McIntosh. Listen to the full conversation with Louise Bradley and then explore others in the Wicked Mind series.
Like many senior leaders, Louise Bradley, past president and CEO of the Mental Health Commission of Canada, had always advocated for mental health, but she was hesitant to talk about her own. It was only when a colleague urged her to publicly share her stories – about growing up in the foster care system and losing a friend to suicide — that she realized the power and impact of being open about her own mental health experience.
When she shared her experience publicly at a conference, a guest approached her after the talk. She shared that she was just about to look at her phone and social media when she heard Bradley’s story. She told Bradley, “‘Wow’- I was just looking at my phone and starting to read Twitter, and then I realized ‘This is not just another CEO talking. [….] She put her phone away and listened to every word, she had tears in her eyes.”
She now feels that leaders of organizations need to show their vulnerability and share their personal struggles with mental health to help make their workplace one in which people feel confident reaching out for help. “You’re being vulnerable and showing that you are human,” she says. “In a leadership position, I think it is one of the most powerful things that I have ever experienced.”
In addition to leaders being more open about their personal experience with mental health, Bradley says that it is incumbent on corporate Canada to provide mental health services, whether in the workplace or the community. She also feels that mental health delivery has to change due to the current challenges experienced by the healthcare system. “There are private companies that are developing new and different innovations, and I really do believe in what they’re doing,” she says.
Mental health diagnoses are rising, with one in three Canadians – or 9.1 million people – affected by a mental illness during their lifetime. There’s a dire need for practitioners that can help, however she calls out the lack of psychiatrists, leaving primary care physicians to diagnose and treat mental health conditions.
As a result, she believes there needs to be more innovation around how mental health support is delivered, in the same way pharmacies are playing a larger role in delivering primary care to Canadians. Pharmacists can now prescribe certain medications, providing vaccinations and imparting critical health information to customers, taking the pressure off primary care doctors.
Some of the innovations in mental health support – and areas that require more focus – include:
Peer support
One way to increase mental health support in the workplace is peer support “Not everybody needs a psychiatrist or a psychologist,” says Bradley. “It could be someone else who has walked a mile in their shoes and has learned some ways of being able to talk and help.” (The topic of Peer Support was also explored by Stephane Grenier and Denis Trottier, both guests on the Wicked Mind pod).
Creating groups and providing them with effective training and support training can be a low-cost and very effective means of assisting employees struggling with their mental health. “We’ve really got to start thinking differently about where and who provides mental health care,” she says.
Suicide prevention
Bradley is a vocal champion for the creation of a national suicide prevention strategy. She says that many groups have identified a need for suicide prevention programming and interventions, and talked about the issue in post-secondary education, where many students fail to get the support they need in the high-stakes, high-pressure setting of academia.
“5,000 people every year die by suicide, and those are the ones that are registered as dying by suicide,” says Bradley, adding that these figures rarely change year to year. “I would be very happy if we could see that being taken more seriously,” she says. “These are senseless deaths that have a huge and lasting impact on so many people.”
The standard for psychological health and safety
Bradley and the Mental Health Commission of Canada team developed the National Standard for Psychological Health and Safety in the Workplace, a framework for employers to create a healthier, psychologically safe workspace. She says that when organizations introduce the standard it has a domino effect, leading employees to become more open to discussing their mental health concerns with friends and family. They also become more confident discussing their challenges at work. “I think [employers] have a very big role and an important one – and it’s important for them to realize that [mental health programs] are a huge investment,” she says.
Despite the work that still needs to be done, Bradley is happy with the progress that has been made thus far.
“Back in 2012, we were just beginning to talk about stigma. And if you needed time off to go for help to a psychologist, you lied about it,” she says. “We have made progress. I don’t think a day goes by now that you turn on the radio or listen to TV that you don’t hear mental health talked about,” she says. “That’s improvement.”
Listen to my conversation with Louise Bradley on the Wicked Mind podcast>>
This blog post is part of a series looking at the state of our mental healthcare system and ways we can create sustainable change to improve quality and outcomes for anyone impacted by mental illness.
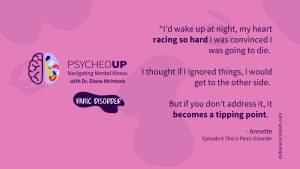
Understanding Panic Disorder: Symptoms, Treatment, Bravery in Asking for Help
Panic disorder, which affects 3.7% Canadians, is “fear gone wrong.” With appropriate therapy and medication, people with panic disorder can keep symptoms in check. Summary of “This is Panic Disorder”, Episode 6 of PSYCHEDUP Podcast.
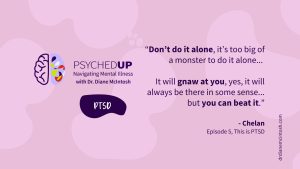
Living with PTSD: A journey from trauma to healing
Post-traumatic stress disorder doesn’t just affect soldiers; it can affect anyone who has experienced trauma. But treatment can help. Chelan shares her story. Summary of “This is PTSD”, Episode 5 of the PSYCHEDUP Podcast.
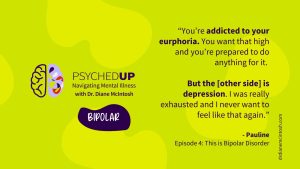
Understanding Bipolar Disorder: The highs, the lows, and the road to equanimity
Bipolar disorder often hides behind depression, making diagnosis a challenge. Pauline navigated years of highs and lows before finding stability. Hear how finally receiving an accurate diagnosis and effective treatment can transform lives for people like Pauline. Summary of “This is Bipolar”, Episode 4 of the PSYCHEDUP Podcast.
