Insomnia

This is Insomnia

A diagnosis of chronic insomnia requires sleep difficulty at least 3 days as week for at least 3 consecutive months.
The only thing worse than an awful night’s sleep, is two awful night’s sleep. And if they keep adding up, it becomes almost impossible to feel like yourself.
In this episode Dr. Diane McIntosh talks about chronic insomnia through the eyes of Allison, a 52-year-old woman who battled sleepless nights for most of her adult life. From waking up exhausted with “baseballs for eyes”, to shying away from socializing because she was so tired, Allison explains what it’s like to live with a disorder that affects 10% of the population.
Dr. McIntosh breaks down the science behind chronic insomnia, while exploring the vicious cycle of poor sleep and declining mental health. She’s joined by psychologist Dr. Randy Mackoff to talk about treatment. From the dangers of self-medicating to the promising new class of medications, this episode provides both hope and practical solutions for anyone trapped in the exhausting world of sleepless nights.
Listen, rate + share Insomnia on your favourite podcast platform:
Thinking of suicide or worried about someone you know? Call or text 9-8-8, toll-free, anytime, for support.

PODCAST GUEST
Dr. Randy Mackoff, PhD
Registered psychologist
Dr. Randy Mackoff is a registered psychologist in British Columbia. He has a private clinical practice where he provides psychological treatment for a wide range of issues, including but not limited to depression, anxiety, PTSD, coping with psychosis, and marital therapy. He is a retired Professor in the Criminology Department at Douglas College and a past Chairperson of the Criminology Department. He is a Clinical Associate in the Clinical Psychology Department at Simon Fraser University, providing clinical supervision to graduate students. He currently consults with law enforcement agencies in Crisis Negotiations, Undercover Operations, Witness Protection, Psychological Support for witnesses, Source Suitability, Major Crimes, Recruiting, and Human Resources. He is a designated Vancouver Police Department Psychologist and represents them at the Major Cities Chiefs Association Psychology meetings. He is the Co-Chair of the Psychology Committee for the Canadian Association of Chiefs of Police (CACP).
More About Insomnia
An insomnia diagnosis requires more than the occasional restless night. It’s a common sleep disorder that makes it difficult to fall asleep, stay asleep, or return to sleep after awakening too early.
While short-term sleep difficulties are common and usually resolve on their own, chronic insomnia is different. It persists for at least three nights per week for three months or more and interferes with how you feel and function during the day.
Chronic insomnia can affect your mood, energy, concentration, relationships, physical health, and overall quality of life. For some, it becomes a cycle of exhaustion, frustration and worry that makes restful sleep feel out of reach.
People with insomnia often experience a combination of nighttime and daytime symptoms.
These may include:
Nighttime symptoms:
- Trouble falling asleep
- Waking during the night and struggling to get back to sleep
- Waking earlier than intended
- Feeling “wired” or alert as soon as you get into bed
- Racing thoughts or worry cycles at night
Daytime symptoms:
- Fatigue or low energy
- Difficulty focusing, impaired memory, or “brain fog”
- Irritability, frustration, or low mood
- Feeling unrefreshed despite time in bed
- Reduced work or school performance
- Avoiding social plans due to exhaustion
- Chronic insomnia is also linked to higher rates of anxiety and depression, and it can worsen existing mental or physical health conditions.
Get checked out by your healthcare provider (HCP) if you’re experiencing chronic insomnia and any of the following:
- Loud, consistent snoring or if you’re awakening through the night gasping for breath. If you sleep alone, so you don’t have someone to complain about your snoring, see your HCP if you’re awakening consistently with a headache or sore throat, and you’re completely exhausted, day and night, despite getting lots of sleep.
- Extremely restless legs (you feel like you must move them) that are preventing you from getting to sleep.
- Persistent symptoms of any mental illness, such as depression or anxiety, that, if treated, could improve the amount and quality of your sleep.
Effective treatment begins with understanding the factors that contribute to poor sleep, such as lifestyle choices, stress, all mental illnesses (especially when anxiety and depression are prominent), pain or chronic medical illness.
Cognitive Behavioural Therapy for Insomnia (CBT-I)
CBT-I is an evidence-based, structured therapy that helps you change the thoughts and habits that keep insomnia going. It focuses on:
- Understanding how sleep works
- Reducing anxiety around sleep
- Restructuring unhelpful thoughts (“I must sleep right now!”)
- Resetting sleep schedules and behaviours
- Breaking the association between the bed and wakefulness.
CBT-I takes commitment, but research consistently shows it can meaningfully improve sleep for many people.
Medication
Medication can play an important role in treating insomnia, particularly when symptoms are severe or linked to another condition, such as depression or PTSD.
- Over-the-counter sleep aids: These are commonly used but often don’t support restorative sleep and can lead to next-day grogginess or other health risks.
- Older prescription options: Benzodiazepines and “Z-drugs” may help, but they carry risks including impairing daytime function, memory problems, falls, and potential dependence, especially if an underlying mental health condition isn’t properly addressed.
- Antidepressants: Some are commonly used to treat insomnia, like trazodone or mirtazapine. While they don’t have the dependence issues listed above, they can cause all of the other side effects associated with benzodiazepines and Z-drugs. Research data does not support their use in chronic insomnia.
- Antipsychotics: These drugs, particularly quetiapine (Seroquel), are commonly prescribed for insomnia. However, they are associated with significant risks, such as a chronic movement disorder called tardive dyskinesia, as well as weight gain and metabolic syndrome. Antipsychotics should NOT be prescribed as a primary insomnia treatment.
Newer, safer options: Dual Orexin Receptor Antagonists (DORAs) are a newer class of medications that are generally very well tolerated and don’t have the same hangover, risk of falls, cognitive issues or dependence risks.
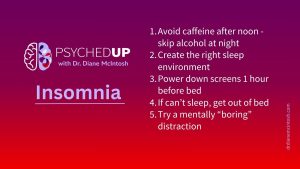
(AKA Sleep Hygiene) These simple strategies won’t cure chronic insomnia on their own, but they create a healthier foundation for sleep:
- Create a calm sleep environment. A cool, dark, quiet room is ideal. Pets are adorable, but they’re not great bed partners.
Use your bed for sleep or sex only. It shouldn’t be a dinner table, theatre or work station.
Limit caffeine after noon and avoid alcohol at night. Both disrupt restful sleep more than many people realize.
Turn off screens an hour before bed. Phones, laptops, and TVs stimulate the brain and delay sleepiness.
- If you can’t sleep, get out of bed. Lying awake teaches your brain that the bed is a place to stay alert. Get up briefly, keep lights low, and return once you feel sleepy again. Don’t eat or use your phone!
- Try a simple mental distraction. Choose something quiet and boring, like alphabetizing U.S. states in your head. These gentle tasks interrupt worry cycles and help the brain drift toward sleep.
Episode Highlights

6:54
Allison and Diane discuss how chronic insomnia can lead to excessive focus on sleep, maladaptive behaviors, and heightened anxiety in the bedroom.

9:18
Diane shares sleep optimization tips.

12:09
Talk therapy for insomnia: Diane and Randy explain Cognitive Behavioral Therapy for Insomnia (CBT-I).

20:18
Self-medication pitfalls.

23:05
Prescription medication overview.
26:06
Allison’s breakthrough: After trying different medications, Allison finds success, achieving 7–9 hours of sleep and feeling truly rested for the first time in years.
Key quotes from the episode
“It’s important to note that
there are financial costs to chronic insomnia. People who have it have higher rates of workplace absenteeism and presenteeism.”
5:15
“I’m trying to not make this sound as bad as it is but there’s really nothing good about not sleeping.” 11:32
“Paradoxically by saying, ‘I just need rest’, they actually fall asleep.” 15:29
“I say boring before bed is best.” 17:25
“People are turning to alcohol, turning to marijuana and using other over the counter medications. And one of the things that happens from that is that sometimes they do fall asleep from that, but they don’t get restorative sleep.” 21:00
Other PSYCHEDUP Episodes
Season 2
Related Posts on Insomnia
Feedback on the Podcast?

Psychiatric Guidance for Optimal Patient Care
Founded by Dr. Diane McIntosh, RAPIDS Health provides timely, effective clinical decision support for mental health diagnosis and treatment. Whether you’re a clinician or someone seeking help, we offer evidence-based, personalized treatment guidance tailored to each individual’s needs.