I'm Lucky You're Here - Collaboration, Leadership & Disruptive Technology are Necessary to Address the Mental Healthcare Crisis - Reflections on Season 1 WickedMind
In Season 1 of Wicked Mind, I was lucky to have conversations with hopeful and pragmatic leaders who have taken urgent action to make change happen. Here are some take-aways from our conversations on the Wicked Mind podcast.

Last year I joined a tennis club, but I’ve never played tennis, except in local school yard courts back in grade 10. I’ve learned that tennis is a really technical and challenging sport and I am, even a year into lessons and regular play, absolutely awful.
Recently, I listened to a group of women playing doubles beside me. After just about every missed shot, a player would say, “I’m so sorry,” in a contrite, almost embarrassed manner. It was a tsunami of sorrys.
When my friends arrived to play, I told them what I’d heard and suggested we stop saying, “I’m so sorry,” when we miss a shot and switch to the self-affirming “You’re lucky I’m here!”
I wanted to turn my frequent bad shots into something that better reflects the experience: we’re here, playing together, learning new skills and building our mental and physical health. As none are confirmed narcissists, my group wasn’t really keen on that statement, but I couldn’t help but think about how I constantly apologize, like many Canadians, for just about everything.
With time, my group’s response to someone’s “I’m sorry,” has become, “I’m lucky you’re here.” The tennis is still meh, but the good vibes keep growing.
As a psychiatrist, I have to say “I’m sorry” an awful lot these days. And, I’m sorry to say, they are highly consequential. “I’m sorry I can’t see you as a patient.” “I’m sorry I can’t get you the medication you need.” “I’m sorry our healthcare system is broken.” “I’m so deeply sorry your child died from an overdose – I wish I could have helped more.”
My professional purpose is now clear: to change that disappointment and heartbreak into something positive. I’m seeking solutions.
Mental illnesses are incredibly isolating. Those suffering often feel hopeless, useless and worthless. The people who love and support them also suffer. No one wants to see their friend, family member or workmate in emotional pain, but we often feel powerless to help. Some of that comes from a lack of education… not knowing how to approach someone who has (or might have) a mental illness.
But even for those who know they need help- they’re asking for help- there is a lack of access to high-quality, appropriate mental healthcare. This hurts them and everyone who cares about them.
Our mental healthcare system is in crisis. For too many Canadians, it is completely inaccessible.
In the series of conversations that make up the first season of Wicked Mind, I spoke with an array of thoughtful, gritty, innovative and compassionate leaders, representing highly diverse areas of healthcare delivery.
Now the CMA’s Past-President, Dr. Alika LaFontaine, spoke about mental models and how systems in crisis represent an opportunity to create meaningful and enduring change. The need to confront dysfunctional mental models is critical, as we work to overcome Canada’s mental healthcare crisis – and it’s at this moment of crisis that strong, confident leadership is needed more than ever before.
Dr. LaFontaine and psychiatrist Dr. Matt Chow both know we need to embrace innovative technology in medicine, yet also recognize that medical mental models can be harsh, inflexible and highly resistant to change. Like me, Dr. Chow is a strong advocate for virtual care and is eager to explore other innovative technologies that support care quality and access.
Both of my medical colleagues expressed understanding and empathy regarding burnout within our profession, which holds a personal meaning for me, inspiring hope.
Alika and several other guests, including Louise Bradley, Stéphane Grenier and Denis Trottier, spoke about the importance of workplace culture and its impact on the overall health and wellbeing of team members. Each shared their own story of a toxic workplace culture and their drive to lead differently.
The Digital Supercluster’s Sue Paish is driven, both personally and professionally, to find and foster the most important new healthcare technologies. Louise Bradley’s entire professional life has been focused on providing compassionate healthcare, when and where it’s needed.
Despite barriers, Denis Trottier and Stephane Grenier spoke about their approaches to helping organizations with robust peer-support programs- and we know social support is a massive protector of mental health. Interestingly, peer support is not new, but making it safe, accessible and scalable is- that’s where they’re making a difference.
Every Wicked Mind guest shared their personal or professional experience with stigma regarding mental illness, and while we have made strides, each acknowledged that stigma still creates a significant hurdle for many.
Scott Elliott, executive director of the Dr. Peter AIDS Foundation, shared experiences that were both instructive and hopeful, as the stigma faced by those living with HIV/AIDS has declined much more than many ever expected. Sadly, despite many successes, that battle continues on many fronts. Scott shared one secret to the success of the Dr Peter Centre- creating a space where everyone feels they belong.
Most memorable for me was the strong, consistent thread of courageous, bold leadership that is strengthened with vulnerability – Louise Bradley and I agree it’s a leadership super-power. These themes tied every conversation together.
After an enlightening, inspiring first season, what’s next for Wicked Mind?
Now that I’ve identified my “I’m sorry” fatigue, especially the painful ones that impact patients and their families, I want to dig deeper into solutions and identify who can make them happen, right now!
My innovative technology, which is called RAPIDS, is focused on supporting those who diagnose and treat mental illnesses.
Just how my team will get RAPIDS to the people who will benefit most; that’s where we’ll go next.
I’m not just speaking up for RAPIDS, but for any innovation, any disruptive technology, that can address the mental healthcare crisis, driving enduring, meaningful change.
And, sorry, no more sorry’s.
We need to be brave. We must challenge the status quo. We must demand from our government leaders and our healthcare leaders what we know is right.
We must collaborate, which requires us to listen.
And, dear listeners, we must lead, wherever we can, with compassion.
Until next time, thank you for being a part of the solution. I’m lucky you’re here!
If you haven’t taken the time to listen to all conversations in #WickedMindPod, you can catch up here.
This blog post is part of a series looking at the state of our mental healthcare system and ways we can create sustainable change to improve quality and outcomes for anyone impacted by mental illness.
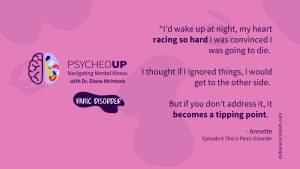
Understanding Panic Disorder: Symptoms, Treatment, Bravery in Asking for Help
Panic disorder, which affects 3.7% Canadians, is “fear gone wrong.” With appropriate therapy and medication, people with panic disorder can keep symptoms in check. Summary of “This is Panic Disorder”, Episode 6 of PSYCHEDUP Podcast.
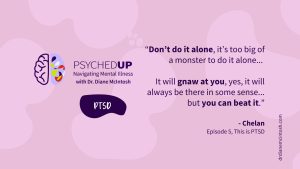
Living with PTSD: A journey from trauma to healing
Post-traumatic stress disorder doesn’t just affect soldiers; it can affect anyone who has experienced trauma. But treatment can help. Chelan shares her story. Summary of “This is PTSD”, Episode 5 of the PSYCHEDUP Podcast.
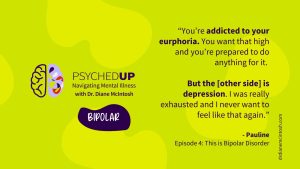
Understanding Bipolar Disorder: The highs, the lows, and the road to equanimity
Bipolar disorder often hides behind depression, making diagnosis a challenge. Pauline navigated years of highs and lows before finding stability. Hear how finally receiving an accurate diagnosis and effective treatment can transform lives for people like Pauline. Summary of “This is Bipolar”, Episode 4 of the PSYCHEDUP Podcast.
