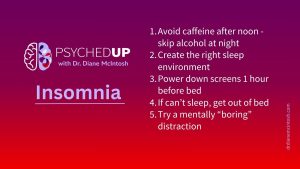
Struggling With Sleep? Here Are My Top Five Tips for Better Rest
I want to share my top five “sleep hygiene” habits that can support healthier sleep. They won’t solve chronic insomnia on their own, but they are essential ingredients for better rest.
Bipolar disorder often hides behind depression, making diagnosis a challenge. Pauline navigated years of highs and lows before finding stability. Hear how finally receiving an accurate diagnosis and effective treatment can transform lives for people like Pauline.
At 62, Pauline has experienced both the highs and the lows of bipolar disorder. Like most people who live with bipolar disorder, she spent years struggling with prolonged periods of depression, which were sometimes followed by periods of mania, an intense high that made her feel like she could conquer the world.
“You elevate yourself to a place of power and privilege — you’re grandiose, you’re generous, you’re flamboyant,” Pauline says. “However, your family sees the greasy underbelly of bipolar, which is irritability, impulsivity, entitlement, selfishness and risk taking.”
Bipolar disorder is best described as a spectrum of disorders, including bipolar I, II and “other specified”. Up to three per cent of Canadians have a bipolar spectrum diagnosis. Bipolar is a mental illness that is characterized by extreme highs and lows, meaning that people with the diagnosis cycle through periods of depression and most also experience periods when they feel elevated, expansive or highly energized, called hypomania (more mild symptoms) or mania.
“When you’re manic, you feel much smarter, sexier, richer and funnier than usual, which is understandably welcomed by individuals who spend most of their time feeling depressed. However, those extremes have a serious downside, as they can lead to uncharacteristic risk taking. Mania is often associated with psychotic symptoms, which usually means holding false beliefs despite clear evidence that those beliefs are false. When manic, common psychotic symptoms include grandiose delusions, such as a belief that you’re a God, or an especially important or powerful person. Sometimes the delusions are paranoid or persecutory, which means a fear that someone is trying to harm you. The presence of psychosis or heightened risk-taking behavior during mania often requires hospitalization, because you’re at risk to yourself or other people,” says Dr. Diane McIntosh, psychiatrist, founder and CEO of RAPIDS Health.
“The lower pole of bipolar disorder is usually called bipolar depression, but it can look just like any other major depressive episode, with sadness, loss of interest and pleasure, and changes in appetite and sleep patterns.”
Because many people go to their doctor with depression symptoms rather than with manic or hypomanic symptoms, they are often misdiagnosed and ineffectively treated, says Dr. McIntosh. “The result is that bipolar disorder is misdiagnosed more than 90 per cent of the time,” she says. “It takes, on average, 10 years and four different clinicians before the right diagnosis is made.”
Pauline was misdiagnosed for decades. Melancholic in her teens, she drifted in and out of depression in her 20s and 30s. It was only after her third child was born and she began taking antidepressant medication that things came to a head.
“That’s when I flipped,” she recalls, and had her first manic episode.
Pauline remembers seeing a man on a park bench with an amputated limb, and feeling as if she could heal him by kissing him. “There’s this sense of having healing powers, that’s delusional, it’s grandiose.” she says.
“Pauline’s description perfectly illustrates the grandiose delusions of bipolar I disorder,” says Dr. McIntosh. “Her psychotic symptoms are so typical of those that occur when you’re manic: most explain that they possess special powers of gifts, like Pauline’s healing powers. When she is well, she would never believe she had those powers.”
Dr. McIntosh explained, “The risk taking associated with mania makes it so dangerous. That might include over spending, inappropriate or unsafe sexual activity, or uncharacteristic alcohol or illicit drug use. Without a correct diagnosis, people often begin to self-medicate with drugs or alcohol.”
For Pauline it was alcohol. “When I wasn’t being adequately treated for my bipolar, I drank,” she says. She recalled the fallout for her family was dramatic. Her children would tape messages to her wine bottles begging her to stop drinking: “’Mommy, you promised to cut back ‘“or “’Mommy, something terrible is going to happen to you,’” she says.
Pauline also began to collect knives. She didn’t plan to hurt anyone—but couldn’t understand what was happening to her. She didn’t understand that she was behaving in a strange or unusual way.
But understandably, her family was concerned. Finally, she was hospitalized under the Mental Health Act. “It very likely saved my life,” she recalls.
In her 40s, Pauline was hospitalized for a month. And she finally had an answer to her bewildering and disturbing symptoms: bipolar disorder.
The biggest challenge in a therapeutic relationship with bipolar patients is helping them to understand what’s happening to them, says Dr. Randy Mackoff, a Vancouver-based clinical psychologist – particularly if they’re manic and detached from reality. He says that when he tells a patient their behavior is harmful to themselves and others, “sometimes they’ll just walk away from that.”
It’s important to look for moments of lucidity to offer guidance. And how the message is delivered is key. “It’s really important to maintain that relationship, not become confrontational,” he says.
Once a person gets a formal diagnosis, there are a number of effective treatments that can help manage symptoms, says Dr. McIntosh. There are two groups of medications that are typically used – mood stabilizers and antipsychotics.
According to Dr. McIntosh, mood stabilizers can be highly effective. One well-known medication is lithium, which is effective in about 30 per cent of patients. It can stabilize a person’s mood and can reduce the risk of suicide, which is higher among people with bipolar. But it can also be challenging to take, because it requires careful monitoring and regular blood work. Lamotrigine and divalproate are other common mood stabilizers.
Antipsychotics are very often prescribed to treat mania/ hypomania and can also help with depression and anxiety symptoms. It’s common to combine mood stabilizers and antipsychotics, as they’ve been found to be most effective when used together, says Dr. McIntosh. Sometimes, antidepressants are used in bipolar disorder because they can be helpful for depression and anxiety symptoms. They are used only when the mood is stabilized with other treatments.
The process of finding the right mix can take time. “My job is to stop the big highs and prevent the lows, helping people to find equanimity,” says Dr. McIntosh. “And that’s a challenge. It takes time to find that right combination, because each brain is unique, and everyone has their own needs.”
Bipolar symptoms sometimes lead to misuse of substances because they can exaggerate the high or numb the low. While people diagnosed with bipolar can have substance use issues, they are too often seen by the healthcare system through the lens of addiction only – the bipolar is missed, with devastating consequences.
Recreational drugs can also confuse the diagnosis. For instance, if someone is habitually using cannabis with a high percentage of THC, it can provoke the onset of bipolar disorder or another psychotic disorders. “It’s very confusing for clinicians, who see a patient using high potency THC and think their symptoms are only related to the drug, when in fact the drug has triggered the onset of another disorder. THC is never a treatment for any psychiatric disorder. Full stop.”
Dr. Mackoff agrees. It’s challenging when you’re treating a patient who is struggling with a psychiatric disorder, such as bipolar, along with substance misuse. “It’s really about having people not become self-loathing because they have been using the substances, but at the same time not encouraging the continuation of the use of substances,” says Dr. Mackoff.
Pauline struggled for years, especially as she enjoyed the feelings of mania. “You’re addicted to your euphoria,” she explained. But once she was properly diagnosed and treated, she came to realize that she never wanted to be hospitalized again. And, the depression was exhausting, and she never wanted those feelings again.”
“I would like to have gotten treatment sooner,” she says. “But I am really lucky. I didn’t really lose anything irreparable. I kept my family, I kept my job, I kept my friends.”
“I was a pain in the butt, but, you know, it could have been a whole lot worse.”
Listen to This is Bipolar Disorder>>
Read transcript of This is Bipolar Disorder>>
Learn more about the PSYCHEDUP podcast>>
This blog post is part of a series looking at the state of our mental healthcare system and ways we can create sustainable change to improve quality and outcomes for anyone impacted by mental illness.
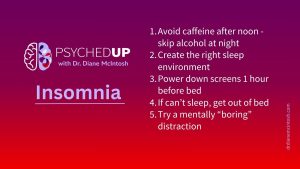
I want to share my top five “sleep hygiene” habits that can support healthier sleep. They won’t solve chronic insomnia on their own, but they are essential ingredients for better rest.

There’s something about flipping the page on the calendar from December to January. For many of us, the beginning of a new year represents a clean slate. So, if you find yourself in the mood to take that time to pause and reflect after the holidays, here are a few tips on making smart New Year’s resolutions.

The holidays can be stressful. Here are a few thoughts on how to make the most of what can be a most wonderful time of the year.
Please provide your contact information in the form below. It helps if you provide enough detail in your message so we can help. We look forward to hearing from you!
Thank you for your message. We will respond to your email promptly.