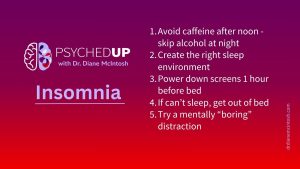
Struggling With Sleep? Here Are My Top Five Tips for Better Rest
I want to share my top five “sleep hygiene” habits that can support healthier sleep. They won’t solve chronic insomnia on their own, but they are essential ingredients for better rest.
Having two or more psychiatric diagnoses at the same time occurs for at least half of those diagnosed with a mental illness. As with other illnesses, it’s important to understand the full picture to find the best treatment.

Lisa’s family doctor diagnosed her with depression but her symptoms didn’t improve with the prescribed antidepressant. Her doctor had her complete some questionnaires that confirmed the depression diagnosis and also determined Lisa had an anxiety disorder, so her doctor suggested she increase the antidepressant dose. Lisa shared this information with her best friend who expressed a strong opinion, stating, “I think you’re being over-medicated. How do you go to your doctor with one diagnosis and leave with two? Are you sure she knows what she’s doing?”
Lisa had started to feel much better soon after her antidepressant dose was increased, but her friend’s comments made her second guess herself and her doctor, so she stopped the antidepressant. Within weeks, her mood and anxiety were much worse, so Lisa went to her local emergency room, where she waited for 12 hours before being assessed. “It was a terrible experience,” Lisa recalled. “I wish I had stuck to the plan I made with my doctor, but I also wish I didn’t need medication at all.”
This fictional story is incredibly common and it speaks to the lack of knowledge regarding the importance of correctly diagnosing and fully treating the symptoms of a mental illness. In this blog, I will unpack the concerns raised by Lisa’s friend and explain why her family doctor ultimately gave her the correct advice.
Psychiatric comorbidity – to have two or more psychiatric diagnoses at the same time – occurs for at least half of those diagnosed with a mental illness.
While Lisa’s friend expressed shock about her having two psychiatric diagnoses at the same time, this is actually pretty much the norm with many illnesses! High cholesterol, diabetes and hypertension commonly co-occur and we don’t ignore any one of them because it seems like too many diagnoses – we know it’s important to treat every disorder to avoid a serious outcome, like a heart attack or stroke. Psychiatric illnesses are no different.
The most common psychiatric comorbidity is major depressive disorder (MDD) co-occurring with an anxiety disorder. About 85% of people diagnosed with MDD have anxiety symptoms. Sometimes, those anxiety symptoms are so consistent, persistent, and impairing that they are referred to as an anxiety disorder.
Anxiety disorders include generalized anxiety disorder, panic disorder and social anxiety disorder. While the DSM-5 no longer categorizes obsessive-compulsive disorder (OCD) and post-traumatic stress disorder (PTSD) as anxiety disorders, both are associated with significant anxiety and both commonly co-occur with MDD.
At some time during their illness, 90% of people diagnosed with an anxiety disorder will have comorbid MDD.
For bipolar disorder (BD), comorbidity is the rule. Studies have found that nearly 70% per cent of people with BD have at least one comorbid psychiatric diagnosis, most frequently anxiety disorders, substance use disorders and ADHD.
Here are the top reasons why the correct diagnosis, including identifying comorbid conditions, is essential.
Lisa’s doctor gave her the best possible guidance by identifying not only the depression but also a comorbid anxiety disorder. Fortunately, antidepressants are prescribed for both anxiety and depression symptoms, when they are distressing and significantly impact an individual’s functioning in their usual roles (e.g., at home, work, school or socially).
By choosing an antidepressant that helps depression and anxiety symptoms and increasing the dose when her symptoms didn’t fully resolve, Lisa quickly started to feel better.
However well-meaning, by undermining Lisa’s confidence in herself and her doctor, her friend’s uninformed comments had a seriously detrimental impact on Lisa’s health, prolonging her journey towards recovery.
Dr. Diane McIntosh is a psychiatrist, innovator, educator, author and speaker. She is a passionate advocate for better mental health care, and a champion for all who suffer from mental health challenges.
See Diane’s other posts on choosing medication.
This blog post is part of a series looking at the state of our mental healthcare system and ways we can create sustainable change to improve quality and outcomes for anyone impacted by mental illness.
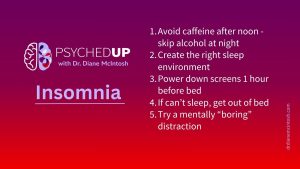
I want to share my top five “sleep hygiene” habits that can support healthier sleep. They won’t solve chronic insomnia on their own, but they are essential ingredients for better rest.

There’s something about flipping the page on the calendar from December to January. For many of us, the beginning of a new year represents a clean slate. So, if you find yourself in the mood to take that time to pause and reflect after the holidays, here are a few tips on making smart New Year’s resolutions.

The holidays can be stressful. Here are a few thoughts on how to make the most of what can be a most wonderful time of the year.
Dr. Diane McIntosh is a psychiatrist, innovator, educator, author, and speaker. She is passionate advocate for better mental health care, and a champion for all who suffer from mental health challenges.
Please provide your contact information in the form below. It helps if you provide enough detail in your message so we can help. We look forward to hearing from you!
Thank you for your message. We will respond to your email promptly.