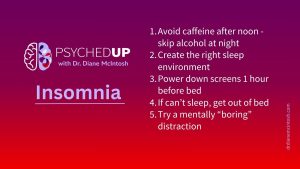
Struggling With Sleep? Here Are My Top Five Tips for Better Rest
I want to share my top five “sleep hygiene” habits that can support healthier sleep. They won’t solve chronic insomnia on their own, but they are essential ingredients for better rest.
Post-traumatic stress disorder doesn’t just affect soldiers; it can affect anyone who has experienced trauma. But treatment can help.
Chelan, now 51, considers herself an average person. “I’m a pretty nerdy, casual, kind of laid-back person — there’s not a lot to me,” says the mother of two, both in their 20s.
But a trauma in Chelan’s past continues to haunt her. Her marriage had broken down, so she told her husband she wanted to separate. His response was horrifying. “He had been getting increasingly irritable but I had no idea what was coming next,” she recalls. “He kicked the door of the guest room open, flicked the lights on, had a rifle pointed at my head, and shots were fired.”
Although the bullets missed her and her then one-year-old daughter, over the next five hours she fought for their lives, as he repeatedly physically and sexually assaulted her. They were lucky to escape. Her husband died by suicide when the police arrived. “I became a single parent in the blink of an eye. My world was irrevocably changed,” Chelan shares.
This terrifying experience left an indelible mark. “I have not had a good night’s sleep in 22 years,” says Chelan. “Every night, I go to bed, I fight for my life. I fight for my child’s life.”
“Every time I close my eyes, it is something I don’t wish on anyone.”
Chelan lives with post-traumatic stress disorder or PTSD. “PTSD is a condition that results from exposure to a terrifying or horrifying, potentially life-threatening event, either as a witness or through direct personal experience,” says Dr. Diane McIntosh, psychiatrist and founder and CEO of Rapids Health.
PTSD commonly includes re-experiencing symptoms, which can make people feel like they’re actually reliving the traumatic event again, says Dr. McIntosh. Re-experiencing comes in many forms, such as intrusive recurrent memories of the traumatic event, nightmares or flashbacks. These symptoms understandably provoke intense distress and anxiety. “Having PTSD can make normal day-to-day life experiences intolerable,” she added.
Dr. McIntosh says that PTSD rarely results from a single traumatic event. “My patients often have a number of traumas in their background, for instance, childhood abuse, often without realizing those experiences are still exerting a heavy toll. Sometimes, one seemingly minor event can be the ‘straw that broke the camel’s back’, provoking the onset of PTSD symptoms. That minor incident might not be severe enough, on its own, to cause PTSD, but it’s enough, on top of a history of traumatic events, to provoke the disorder .” she adds.
Traumatic events, like any scary situation, provoke the nervous system to go into overdrive to protect us from harm. It’s called the ‘fight or flight response,’ says Dr. McIntosh. “There’s increased heart rate and blood pressure and more blood flows to your muscles so you can run. You’re hyper-alert, you’re ready to act. With PTSD, that fight or flight response doesn’t turn off. With time, this can lead to actual structural and functional brain changes that maintain the PTSD symptoms.
Chelan endured years of frightening symptoms – horrible nightmares and daily anger, fear, anxiety and hypervigilance—before she got a diagnosis.
People with PTSD experience a wide range of distressing symptoms, says Dr. McIntosh. These include those intrusive re-experiencing symptoms as well as avoidance of people, places and activities that might trigger memories of the event, irritability, angry outbursts, and behaving recklessly or in a self-destructive manner. Problems with excessive alcohol or recreational drug use are common.
“Everyone with PTSD has trouble sleeping,” says Dr. McIntosh. In Chelan’s case, “the nightmares were unstoppable – and I’d always been a very happy person,” she says. “I didn’t want any contact with people, I didn’t want to live the way I was living.”
Dr. Randy Mackoff, a Vancouver-based clinical psychologist, explains that PTSD risk stems from exposure to the traumatic event — how personal it was, the nature of the event, and how life-threatening it was. But early life experiences of trauma, which can include physical, sexual or emotional abuse or living in chaos or neglect, increases the risk of eventually developing PTSD, explains Dr. Mackoff.
A form of cognitive behavioral therapy, called prolonged exposure, can be very effective in treating PTSD. The therapy involves helping patients, in a very safe environment, to recall all of their thoughts and feelings associated with the trauma, over and over and over again, until they become habituated to the fear they provoke. Other aspects of therapy involve learning new coping strategies to conquer the fear that arises when reliving stressful memories, says Dr. Mackoff.
Another treatment approach, called Eye Movement Desensitization (EMDR), is a psychotherapy technique that may also help treat PTSD. During EMDR, “a person is asked to recall the traumatic event while at the same time moving their eyes back and forth,” says Dr. Mackoff. “For some people, it can be very effective.”
While talk therapy can be very effective, in some cases medications are required.
Antidepressants can be extremely helpful for some patients diagnosed with PTSD, says Dr. McIntosh. “Sometimes, when symptoms are severe and impairing, I also add an antipsychotic medication. The name ‘antipsychotic’ is a misnomer that can provoke fear,” she adds, “but these medications are really effective for the treatment of depression and other disorders that don’t typically include psychotic symptoms, including PTSD.” Because nightmares are so common, disturbed sleep is an issue for virtually every patient. Medications can be very important to help patients get to sleep, stay asleep and have a rejuvenating sleep.” Additionally, says Dr. McIntosh, specific sleep medications can help to break the nightmare cycle.
As with other psychiatric disorders, self-medicating your symptoms with alcohol or cannabis is not recommended, including for managing your sleep symptoms. Alcohol and cannabis for sleep are “not restorative,” explains Dr. Mackoff.
PTSD can be a really difficult disorder to treat, especially when the diagnosis hasn’t been recognized for years. Unfortunately, that’s not uncommon, says Dr. McIntosh, adding, “A delay in diagnosis makes determining the most effective therapy and finding the right medication, which already takes time and a great deal of trial and error, even more challenging.” Chelan agrees. “I’m not going to lie. It was a good five years of ups and downs and pill changes and different therapies before I knew I was on the right path,” she shared.
“I was in and out of psychiatric wards. It wasn’t an easy journey, but those hospital visits were there to save me,” Chelan recalls. “It wasn’t perfect, it wasn’t shiny, but I could see the light at the end of the tunnel that everything that we had done, the treatments, the medication, the therapy, was working.”
In the end, Chelan persevered. “I just had to trust that I could get there. I needed to dig deep, look at the big picture, and trust in the process. Because I wanted to wake up, see my children grow up, I did it.”
“I don’t have as many flashbacks, and I’ve learned to live with my nightmares. If you can just find the silver lining in anything, it makes life worth living. It’s very important, for me, to find the happiness.”
To anyone experiencing what Chelan has, she offered this message: “It will pass, the memories will fade, it does become liveable, and eventually the liveable becomes happiness.”
This blog post is part of a series looking at the state of our mental healthcare system and ways we can create sustainable change to improve quality and outcomes for anyone impacted by mental illness.
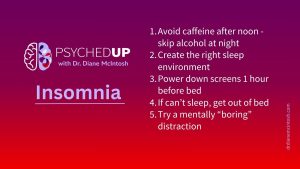
I want to share my top five “sleep hygiene” habits that can support healthier sleep. They won’t solve chronic insomnia on their own, but they are essential ingredients for better rest.

There’s something about flipping the page on the calendar from December to January. For many of us, the beginning of a new year represents a clean slate. So, if you find yourself in the mood to take that time to pause and reflect after the holidays, here are a few tips on making smart New Year’s resolutions.

The holidays can be stressful. Here are a few thoughts on how to make the most of what can be a most wonderful time of the year.
Please provide your contact information in the form below. It helps if you provide enough detail in your message so we can help. We look forward to hearing from you!
Thank you for your message. We will respond to your email promptly.