Struggling With Sleep? Here Are My Top Five Tips for Better Rest
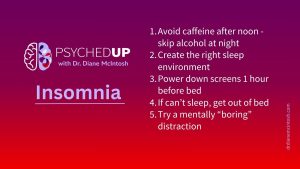
I want to share my top five “sleep hygiene” habits that can support healthier sleep. They won’t solve chronic insomnia on their own, but they are essential ingredients for better rest.
We need to support overloaded clinicians – GPs, nurse practitioners and psychiatrists – by providing them with the tools necessary to deliver more effective, personalized and efficient mental healthcare. That’s the message Dr. Diane McIntosh, Founder and Chief Medical Officer at RAPIDS Health, shared with attendees at Reboot’s 23rd annual health care summit in Vancouver.
This post is a summary of that presentation.
Many Canadians suffering from a mental illness are untreated, under-treated, misdiagnosed, or have inadequate care.
Most people struggling with a mental illness are treated, initially or primarily, by their family doctor or nurse practitioner. This is appropriate because primacy care practitioners (PCPs) should be the most accessible providers and also have a holistic understanding of their patient’s health and wellness. Unfortunately, millions of Canadians don’t have a primary care provider.
Additionally, mental illnesses are challenging to diagnose, because psychiatry lacks objective measures, such as blood tests or brain scans, to support diagnostic accuracy. Finding the right treatment is essential, and that is predicated on having an accurate diagnosis. However, even with the right diagnosis, the process of finding an effective, tolerable treatment can be extremely frustrating, for patients and providers, because it often requires a great deal of trial and error. All of the available treatments work, but they don’t work for every individual. The science of psychiatry is rapidly advancing, but medical education that adequately integrates and reflects those scientific advancements is lacking.
Here are some of the challenges associated with psychiatric diagnosis and treatment:
Dr. McIntosh acknowledges that hoping for major improvements in mental healthcare delivery is a tall order at a time when clinicians are experiencing a high rate of burnout following the pandemic. She says that 60% of doctors surveyed in November 2023 reported their mental health had worsened during the pandemic and 53% experienced high levels of burnout. 60% were planning to reduce their hours or leave the profession in the next 5 years.
“We need to make things easier for our healthcare providers,” she said.
Dr. McIntosh points out that, because of this complexity and the hard-to-close education gap, many healthcare providers fail to correctly diagnose psychiatric disorders, with misdiagnosis rates between 66% and 98% in primary care.
“Bipolar disorder, for example, is the most commonly missed diagnosis. It can take four clinicians and more than ten years before the correct diagnosis is made,” she says. This is compounded by a lack of access to family physicians, nurse practitioners, and psychiatrists.
Medication is an important tool for many patients diagnosed with a mental illness. Personalizing treatment- finding the right medication for the right person at the right time- is critically important. All medications can have side effects, including impaired sexual function, weight gain, and others. New medications are not necessarily more effective in managing symptoms but they are often better tolerated, so patients are more likely to take them. No drug will work if it’s not taken. Many clinicians aren’t familiar with newer treatments and access may be limited by private or public health insurers.
As a result, many Canadians with psychiatric disorders struggle for years with symptoms and side effects of their medication, leading to treatment discontinuation, illness progression, prolonger suffering, multiple relapses, functional impairment and significant financial burdens related to work absence or the inability to work.
Having a mental illness also increases patients’ risk of developing a chronic physical illness, such as heart diseases, diabetes, obesity or other inflammatory illnesses – and the presence of one of a serious physical illness increases the risk of developing a mental illness, such as bipolar disorder or depression, says Dr. McIntosh. The human costs to the patient, in terms of suffering and functional impairment, and the financial burden on our healthcare system and employers, are enormous.
We must improve diagnostic accuracy, improve psychiatric education for doctors, nurses, pharmacists and all healthcare providers, and heighten awareness regarding psychiatric stigma, which continues to be a reality in medicine, says Dr. McIntosh.
Here are some steps we can take, now, to make this happen:
The key now is to raise the bar for mental healthcare. “Our goal at RAPIDS is to revolutionize mental healthcare through innovation, education and compassion,” says Dr. McIntosh.
We are judged as a society by how we treat our most vulnerable members. We’re judged as a profession by how we treat our most vulnerable patients. The time to act in now.
To learn more, follow RAPIDS at rapidshealth.com. Dr. McIntosh and the RAPIDS team will update the site with information regarding when the RAPIDS system will be available to GPs and other decision makers.
This blog post is part of a series looking at the state of our mental healthcare system and ways we can create sustainable change to improve quality and outcomes for anyone impacted by mental illness.
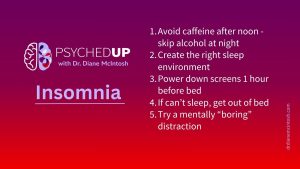
I want to share my top five “sleep hygiene” habits that can support healthier sleep. They won’t solve chronic insomnia on their own, but they are essential ingredients for better rest.

There’s something about flipping the page on the calendar from December to January. For many of us, the beginning of a new year represents a clean slate. So, if you find yourself in the mood to take that time to pause and reflect after the holidays, here are a few tips on making smart New Year’s resolutions.

The holidays can be stressful. Here are a few thoughts on how to make the most of what can be a most wonderful time of the year.
Please provide your contact information in the form below. It helps if you provide enough detail in your message so we can help. We look forward to hearing from you!
Thank you for your message. We will respond to your email promptly.