Struggling With Sleep? Here Are My Top Five Tips for Better Rest
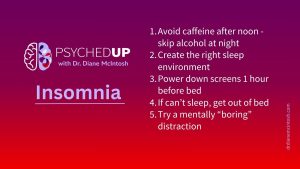
I want to share my top five “sleep hygiene” habits that can support healthier sleep. They won’t solve chronic insomnia on their own, but they are essential ingredients for better rest.
Like all medications, taking an antidepressant may come with unpleasant side effects. Fortunately, most are mild and short-lived, such as nausea or headache, and can often be avoided by starting at a low dose and increasing slowly.

Unfortunately, some antidepressants have side effects that may be more severe and persistent, especially weight gain, sexual problems or an inability to feel a normal range of emotions.
However, there are some antidepressants that are much less likely to cause these side effects.
When depression and anxiety symptoms have fully resolved and the decision is made to stop the treatment, some patients report experiencing very unpleasant side effects, called “discontinuation symptoms.”
Two older antidepressants, paroxetine (Paxil) and venlafaxine (Effexor), are particularly problematic, sometimes provoking flu-like symptoms, intense emotions (e.g., anxiety, mood lability), and electric-shock sensations, when discontinued.
For these two antidepressants, in my clinical experience, it doesn’t seem to matter how slowly they’re discontinued (even over months), they can still provoke these symptoms.
This is why most of my psychiatrist colleagues abandoned their use years ago, choosing to prescribe antidepressants with better short- and longer-term side effect profiles.
While many antidepressants can provoke discontinuation-related symptoms, they are rare in my practice because I avoid the worst offenders, inform my patients, and ask them to keep me in the loop if they decide to stop their treatment, so I help manage the symptoms if they arise.
Distressingly, there is a persistent belief, fueled by inaccurate reporting, that every patient is at high risk of discontinuation symptoms and that every antidepressant carries the same risk. This misinformation heightens treatment fear for individuals who are already anxious and really need help.
Headlines regarding psychiatric treatments tend to focus on the worst possible outcomes.
Some are frankly dishonest.
Online and print articles have reported on a recent review (Lancet Psychiatry. 2024 Jul; 11(7):526-535) of 79 scientific papers, stating that 1 in 3 people who stop taking an antidepressant experience discontinuation symptoms. While the study did find that 31 per cent of the subjects endorsed one or more discontinuation symptoms, 17% of participants had discontinuation symptoms after stopping a placebo. The researchers concluded that 15% per cent of subjects experienced antidepressant-related discontinuation symptoms and just 2.8% experienced severe discontinuation symptoms.
Another important consideration: more than 75% of patients stop their antidepressant before they have fully recovered, so there are times when what is labeled “discontinuation symptoms” is actually a relapse or due to residual symptoms of depression. Depression relapse can be delayed by weeks or even several months after an antidepressant is discontinued.
If you’re struggling with depression or anxiety and your doctor or nurse practitioner (NP) suggests you consider an antidepressant, it’s possible to reduce the likelihood of both short- and long-term side effects and substantially reduce the risk of discontinuation symptoms, if and when it’s time to stop your antidepressant.
Here are my 7 top tips for optimizing your antidepressant experience:
Dr. Diane McIntosh is a psychiatrist, innovator, educator, author and speaker. She is a passionate advocate for better mental health care, and a champion for all who suffer from mental health challenges.
This blog post is part of a series looking at the state of our mental healthcare system and ways we can create sustainable change to improve quality and outcomes for anyone impacted by mental illness.
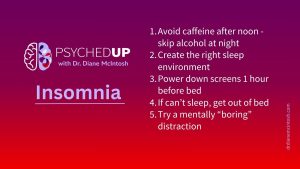
I want to share my top five “sleep hygiene” habits that can support healthier sleep. They won’t solve chronic insomnia on their own, but they are essential ingredients for better rest.

There’s something about flipping the page on the calendar from December to January. For many of us, the beginning of a new year represents a clean slate. So, if you find yourself in the mood to take that time to pause and reflect after the holidays, here are a few tips on making smart New Year’s resolutions.

The holidays can be stressful. Here are a few thoughts on how to make the most of what can be a most wonderful time of the year.
Dr. Diane McIntosh is a psychiatrist, innovator, educator, author, and speaker. She is passionate advocate for better mental health care, and a champion for all who suffer from mental health challenges.
Please provide your contact information in the form below. It helps if you provide enough detail in your message so we can help. We look forward to hearing from you!
Thank you for your message. We will respond to your email promptly.