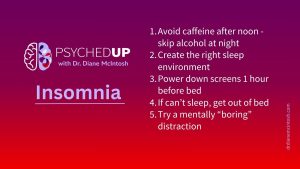
Struggling With Sleep? Here Are My Top Five Tips for Better Rest
I want to share my top five “sleep hygiene” habits that can support healthier sleep. They won’t solve chronic insomnia on their own, but they are essential ingredients for better rest.
For many people living with severe mental illnesses, recovery is a hard-won battle. It can take years of the right treatment, talk therapy, social support, and persistence. But once the worst is behind them, recovery can come with an unexpected challenge: staying well.
Everyone who’s endured a serious mental illness is eager to recover their sense of normalcy. More than anything, they want the return of their best quality of life. But during the early days of symptom remission — of wellness — my patients very commonly report a lingering fear that their illness will return. It’s like they’re always looking over their shoulder, worried their symptoms will sneak up and clobber them again when they least expect it.
Likewise, their primary supporters — friends and family members who have lived through their journey through illness and into recovery with them — often describe the same fear. It’s really difficult to feel free of illness when you’re constantly fearful it will return.
But with time, most people start to feel safe in their wellness. They stop looking over their shoulder and start facing their future with confidence. This is everyone’s goal — getting back to work, back to love, back to life.
Unfortunately, that’s not where the recovery story always ends.
I feel like I must always walk a tightrope when it comes to supporting my patients who are well. I want to encourage them to live their life as a perfectly well person, but I never want them to lose their healthy respect for their illness, which is a part of them. That’s because if you don’t respect the illness and acknowledge its existence, you can start to lose your power to control it.
It often happens like this: after a difficult period of illness, which might have taken lots of treatment trials and years to overcome, my patient is finally well. They’re happily living their life, taking their medication and maintaining a healthy balance of self-care and social engagement. They are well. But over time, and often with exposure to other opinions (e.g., Dr. Google, their mother-in-law or their beautician), they begin to wonder, Was it really that bad? Do I really need this medication? Maybe I can stop and I’ll be fine now?
These questions are human. They don’t reflect denial or failure, they reflect hope.
But from scientific research and my 25 years of clinical experience the reality is stark and clear. When someone loses respect for their serious mental illness, especially if it was difficult to treat, recurrent or involved psychosis, relapse commonly follows. And sadly, the symptoms are usually more difficult to treat.
I want every one of my patients to be free of illness. But I also want them to remember what they’ve been through. Respecting your illness doesn’t mean living in fear. It means staying grounded in what you’ve learned, trusting your team, and recognizing the importance of consistency, especially when it comes to treatment.
In our PSYCHEDUP episode on psychosis, we shared the story of “John” (alias used to protect his identity), a patient who relapsed multiple times after stopping his medication. Each time, he held onto hope that maybe it was no longer needed. But each time, the illness returned.
Eventually, John made a powerful decision: to stop fighting the idea of lifelong treatment and embrace the reality that staying well was worth the trade-off.
“I’ve come to the realization that I’m going to have to take this medication forever,” he told me. “Every time I try to stop, I relapse. And I don’t know how many more relapses I can take.”
That kind of honesty takes incredible strength. Today, John is thriving. He has a loving partner, a fulfilling career, and a life he never imagined possible. He still lives with the memory of what he’s been through, but he also lives with hope and that’s what truly matters.
Recovery doesn’t always mean a perfect cure. It means living your best life, with the right support, structure, and self-compassion.
As John said so powerfully:
“Even a 95% cure is a tremendous improvement. It doesn’t have to be this way. There is help.”
It’s also important to advocate for yourself. If you’re unhappy with your treatment side effects, even if a medication is working, please speak up — repeatedly, if necessary — and ask your healthcare provider to offer you other options.
If you’re caring for someone with psychosis or navigating it yourself, I encourage you to listen to the full podcast episode on PSYCHEDUP. We explore what psychosis really is, the challenges it presents, and how compassionate, evidence-based care can make a difference.
If you find the episode helpful, consider sharing it with someone who might benefit from hearing it. Leaving a rating or review can also help more people discover the podcast and remind them that they’re not alone.
With gratitude,
Diane
Diane McIntosh, MD, FRCPC
Psychiatrist, Founder and CEO RAPIDS Health, Host PSYCHEDUP
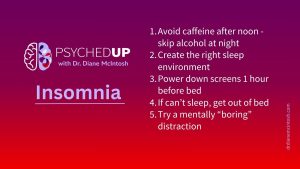
I want to share my top five “sleep hygiene” habits that can support healthier sleep. They won’t solve chronic insomnia on their own, but they are essential ingredients for better rest.

There’s something about flipping the page on the calendar from December to January. For many of us, the beginning of a new year represents a clean slate. So, if you find yourself in the mood to take that time to pause and reflect after the holidays, here are a few tips on making smart New Year’s resolutions.

The holidays can be stressful. Here are a few thoughts on how to make the most of what can be a most wonderful time of the year.
Please provide your contact information in the form below. It helps if you provide enough detail in your message so we can help. We look forward to hearing from you!
Thank you for your message. We will respond to your email promptly.